LECTURES
Currently, in the structure of mortality in the Russian Federation and a number of other countries, oncological diseases occupy a leading position among other causes. Melanoma of the skin is one of the most aggressive malignant tumors, with rapid progression, often leading to death in a fairly short time. Early detection and rationally organized refferral of patients with diagnosed skin melanoma in primary health care settings is aimed at reducing morbidity and mortality from malignant diseases, and improving the quality of life of patients. Research results suggest that the increased incidence of skin melanoma is due to both overdiagnosis. and an increase in the alertness of doctors and the population in relation to pigmented skin formations. The article discusses the proven risk factors for the development of skin melanoma, since this disease is potentially reversible. Attention is paid to modern clinical methods for predicting the course of skin melanoma. The review article examines computer-based methods for screening and diagnosing skin melanoma, applicable in primary health care settings. A separate section is devoted to dermatoscopy or epiluminescence microscopy, which refers to the study of pigmented skin lesions using surface microscopy. A list of studies is presented in case of suspicion of a malignant neoplasm of the skin / melanoma of the skin in a patient who sought medical help at a medical and prophylactic institution. The significance of the criteria of the ABCDE algorithm, the “Argenziano” algorithm in the study of pigmented skin lesions with further analysis of the results by artificial intelligence for decision-making is discussed.
Neurofibromatosis type 1 is the most common autosomal dominant tumor syndrome. The prevalence of the disease is 1 in 3000 people. Neurofibromatosis type 1 is characterized by the gradual appearance of signs of the disease and pronounced clinical polymorphism from erased and atypical forms to severe classical manifestations. The review is devoted to the consideration of diseases, the manifestations of which are significantly similar to neurofibromatosis type 1, and therefore, molecular diagnosis of the disease is an important method for differential diagnosis. To make a diagnosis of neurofibromatosis type 1, it is necessary to find mutations in the NF1 gene using sequencing. In 10% of cases, neurofibromatosis type 1 is caused by large deletions of the 17q11.2 locus, therefore, multiplex ligation-dependent probe amplification is also necessary. Typically, the initial manifestations of neurofibromatosis type 1 are multiple café-au-lait spots, which may be the only external signs of the disease for many years. Therefore, patients with neurofibromatosis type 1 may be mistakenly diagnosed with diseases for which these pigmentary changes are characteristic: Bloom, LEOPARD, Carney, Costello, Cowden, Legius, Nijmegen, Noonan, Peitz-Jägers, Silver-Russell, cardio-facio-cutaneous syndromes. The detection of subcutaneous tumors can become the basis for an incorrect diagnosis of the clinically similar Legius syndrome and multiple endocrine neoplasia. In addition, multiple lipomas are specific manifestations of Madelung or Dercum lipomatosis, familial angiolipomatosis, the etiology of which is considered unknown. Therefore, I assume that these diseases are atypical forms of neurofibromatosis type 1, since a number of authors have described the identification of mutations in NF1 gene in patients with multiple lipomatosis. Therefore, it is important to widely introduce into clinical practice the possibility of molecular genetic identification of the disease in order to identify cases of neurofibromatosis type 1 that do not meet the diagnostic criteria adopted by the NIH. It is promising to create a panel for the study of all genes, mutations in which can cause manifestations similar to neurofibromatosis. Early diagnosis of the disease is necessary for timely initiation of treatment and prevention of severe manifestations, since effective methods of antitumor therapy of neurofibromatosis type 1, such as inhibitors of mitogen-activated kinase, are being introduced into clinical practice.
REVIEW ARTICLES
Chronic kidney disease is a risk factor for other organ disease. People with kidney disease have an increased risk of developing and dying from cardiovascular disease, and there is also evidence that the risk of cancer and cancer mortality may be increased in people with chronic kidney disease. Chronic kidney disease and malignant neoplasms are interconnected in both directions: cancer can cause damage to the kidney tissue directly or indirectly through the side effects of cancer treatment. In turn, chronic kidney disease, on the contrary, can be a risk factor for the development of malignant neoplasms. In addition, both pathological processes can share common risk factors. Chronic kidney disease can result from the use of chemotherapy drugs. Many of the existing and recently developed cancer chemotherapeutic agents are nephrotoxic and can contribute to renal dysfunction, which often manifests itself in terminal cancer. To date, therapeutic interventions to combat the progressive growth of cancer can accelerate the progression of chronic kidney disease. The article provides data on the interaction of chronic kidney disease and the development of malignant neoplasms. The nephrological aspects of the clinical picture of oncological diseases are considered. The mechanisms of the negative effect on the renal tissue of anticancer drugs — cisplatin, ifosfamide, methotrexate and cyclophosphamide — are discussed. Given the link between kidney disease and the development and treatment of cancer, the review article highlights the importance of interdisciplinary collaboration between oncologists and nephrologists to predict and prevent nephrotoxic effects of cancer chemotherapy, and as new treatments for malignant neoplasms are introduced, proper diagnosis and treatment of emerging malignancies is required. new renal toxic effects.
The review provides data on severe bronchial asthma. Frequent exacerbations of asthma significantly reduce the quality of life of patients, cause disability, disability and death. The heterogeneity of severe bronchial asthma fits into the concepts of phenotype and endotype, the identification of which in clinical practice has limitations, but is necessary for personalized therapy. Analysis of the literature reflecting experience in patient data management is needed to form holistic perceptions of severe bronchial asthma and develop ways to optimize therapy.
ORIGINAL ARTICLE
Aims. To study the CYP2C19(681A/G) polymorphism among the population of the Trans-Baikal Territory in comparison with data in other regions of Russia and the world. Materials and methods. The study involved 132 people (81 women and 53 men). The median age was 47 (18; 72) years. Genotyping of the 681G/A polymorphic locus of the CYP2C19 gene was performed by polymerase chain reaction. Results. The prevalence of CYP2C19(681G/G) was 105 people (79.6%), CYP2C19(681G/A) — 25 people (18.9%) and CYP2C19(681A/A) — 2 participants (1.5%). Allele A of the CYP2C19 gene in position 681 was found in 14.2%. Allele A is less common in the population of the Trans-Baikal Territory, compared with Asians (China, p <0.001; Japan, p = 0.015) and did not differ in prevalence from Native Americans, Hispanics, African Americans, residents of Moscow, Voronezh, Irkutsk regions and Sakha-Yakutia. CYP2C19(681A/A) was more common in the Asian population than among the Transbaikalians, p = 0.003. The prevalence of the CYP2C19(681A/A) genotype did not differ between the population of the Trans-Baikal Territory, African Americans, Caucasians, and the population of the Moscow and Voronezh regions. Conclusions. The prevalence of the allele A in the population of the Trans-Baikal Territory was 14.2% and was comparable to the Caucasians, but less common than in the Asian population. The prevalence of the CYP2C19(681A/A) was 1.5%, which was consistent with world data among Caucasoid populations and was less common than in Asians.
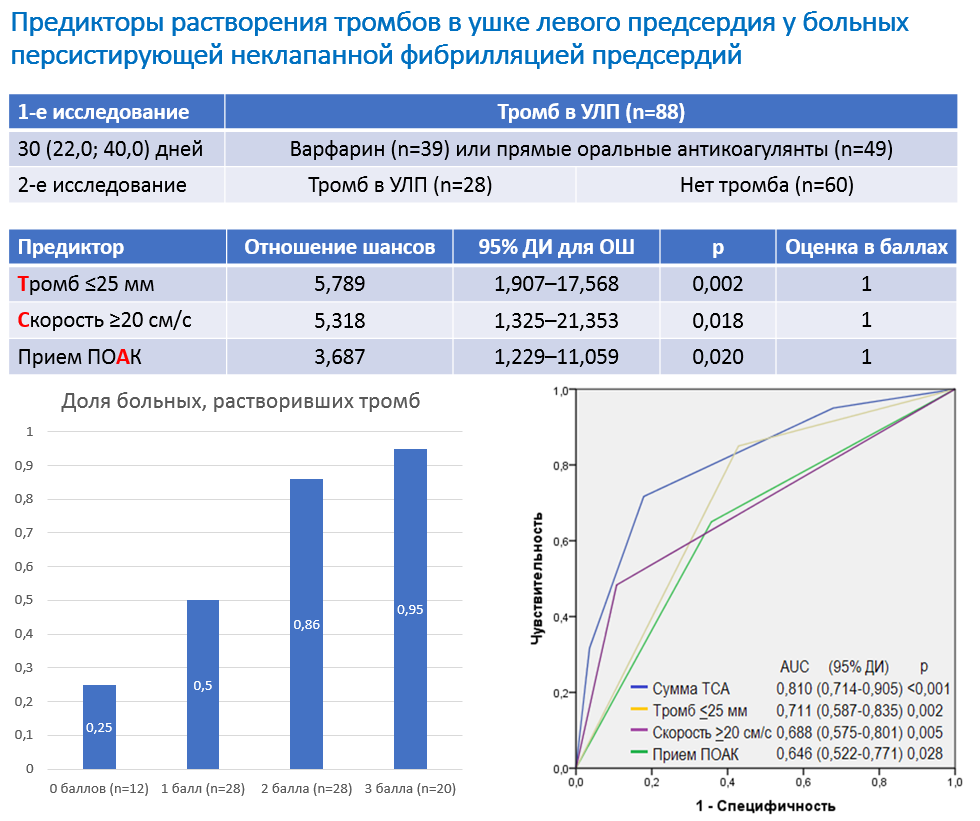
The aim of this study is to identify factors influencing the likelihood of the thrombus dissolution in the left atrial appendage in patients with persistent nonvalvular atrial fibrillation. Material and methods. A repeated transesophageal echocardiography was performed in 88 patients with persistent nonvalvular atrial fibrillation and with the left atrial appendage thrombus at the first transesophageal echocardiography. Results. The second transesophageal echocardiography was performed on average 30.0 (22.0; 40.0) days after the first one, the thrombus dissolution in the left atrial appendage was revealed in 60 (68.2%) patients. The multivariate logistic regression analysis showed that the chances of the thrombus dissolution increased by 5.789 (1.907–17.568) times with the thrombus size not more 25 mm, by 5.318 (1.325–21.353) times with the left atrial appendage emptying flow velocity not less 20 cm/s and 3.687 (1.229–11.059) times when prescribing the direct oral anticoagulants, and not warfarin. Combination of two or more factors give the probability of the thrombus dissolution of more than 89.6%. Conclusion. The probability of the thrombus dissolution in left atrial appendage in patients with persistent nonvalvular atrial fibrillation increases with a small thrombus size, a high the left atrial appendage emptying flow velocity, and if direct oral anticoagulants were prescribed.
The article is devoted to the development of the level of communicative competence of future doctors and the peculiarities of professional communication with patients. The basis of the work were the questions of determining the speech behavior of a doctor in one of the most difficult communicative situations — the situation of delivering bad news. Based on the material of real recordings of doctors’ speech, the analysis of risky communicative steps in the communication between the doctor and the patient is carried out, the most effective ways of implementing the doctor’s speech tactics in the situation of bad news are determined. Conclusions are drawn about the need to improve the level of professional communication of doctors and to train medical students in the communication skills of delivering bad news.
ANALYSIS OF CLINICAL CASES
Hypotension is often in chronic heart failure patients. It has various reasons, including a decrease in the pumping function of the heart, medications, altered vasoreactivity associated with concomitant diseases (for example, diabetes mellitus). There are no universal criteria for assessing the severity of hypotension. Its prognosis significance has not been studied well. It is difficult to select and titrate the drugs recommended for treatment of heart failure, so that the prescribed therapy compensates the patient and does not cause the development of side effects. Step–by–step algorithms for prescribing and correcting drug therapy for heart failure patients with hypotension have been developed. This article presents a clinical case of management of a patient with severe hypotension and chronic heart failure with a reduced left ventricular ejection fraction.
Aortic valve replacement was performed the patient with congenital heart disease (bicuspid aortic valve) in 25 years. In 13 years, after a viral infection, there was a decompensation of chronic heart failure with reduced ejection fraction to 19%. Against the optimal drug therapy, heart failure persisted III– IV functional class with 4 hospitalization during a year. Despite the indications for cardiac resynchronization therapy, a system for modulating cardiac contractility was implanted, after which there was no improvement in clinical symptoms, there were frequent decompensations up to. In order to prevent the progression of the disease and improve the prognosis, despite hypotension, sacubitril/valsartan was prescribed, against which it was possible to compensate the patient and achieve a stable course of chronic heart failure without the need for hospitalization for 9 months. This case report suggest that additional clinical researches are necessary to study the possibility of prescribing of small doses of sacubitril/valsartan in patients with hypotension and heart failure to reduce the severity of clinical symptoms and to improve the prognosis.
Lyme disease (tick-borne borreliosis) is an infectious vector-borne natural focal disease that tends to a chronic and recurrent course with a predominant damage to the skin, nervous system, musculoskeletal system and heart. Cardiac features is manifested, as a rule, by a involvement of the conducting system as varying degrees of atrioventricular block, Bundle–branch block, dysfunction of the sinoatrial node. In case of untimely diagnosis and etiotropic treatment of tick-borne borreliosis, chronic lesions of the cardiac conduction system may occurs and implantation of a pacemaker may be required.
ISSN 2411-6564 (Online)