REVIEW ARTICLES
Most patients with arterial hypertension require more than one antihypertensive drug for blood pressure target achievement. Some patients are recommended for a multi-pill antihypertensive regimen, others — treatment with fixed dosed combinations in one tablet. Analysis of elibrary and PubMed publications in the period mostly from 2014 to 2024 concerning the choice of two-component combined antihypertensive agents containing renin-angiotensin system inhibitor and diuretic or calcium channel blocker, revealed that fixed-dose combinations (FDC) use and taking one tablet once a day improves adherence to treatment and facilitates blood pressure control. Although the cost of FDC containing the renin-angiotensin-aldosterone system inhibitor and a thiazide/thiazide-like diuretic or calcium channel blocker is in most cases higher than the same drugs taken separately, the use of fixed combinations, increasing patient adherence to therapy, has clinical advantage in terms of the effectiveness of lowering blood pressure, which confirms their economic feasibility. On the other hand, the use of free combination therapy in two different tablets, when taken separately during the day, can sometimes provide a more sustained antihypertensive effect over 24 hours. Evidence of the effectiveness of blood pressure control for FDCs is often extrapolated from data on free combinations. In addition, FDCs are characterized by less detection of possible ineffectiveness of one of the components. The range of FDCs and the dosage ratios of the components presented in them is gradually expanding, but the choice among free combinations is still wider. In addition, the list of vital and essential drugs (VED) for 2024 does not contain FDCs for antihypertensive drugs, which excludes the possibility of free receiving them on a preferential basis and gives the opportunity for the manufacturer to set prices for them. Despite the fact that recently the scientific community has recommended the use of FDC antihypertensive drugs as initial therapy due to better compliance with the regimen, and therefore clinical effectiveness and economic feasibility, it cannot be said that there is no space left for free combinations of antihypertensive drugs in the treatment of arterial hypertension. The choice of doctor, frequency of prescription, share of purchases of the FDCs in the Russian Federation, review of their consumption requires further analysis.
Chronic non- infectious diseases represent an important medical and social problem for the healthcare system. Optimal pharmacotherapy is not always effective enough, and the use of surgical treatment methods is not possible in all patients. In addition, an important link in the comprehensive management of such patients is dosed physical activity, however, in most of them, low exercise tolerance does not allow them to exercise, starting a vicious circle that leads to a decrease in the functional reserve of the body. In this case, the use of non-pharmacological treatment methods, for example, enhanced external counterpulsation, may be useful. This review is devoted to the analysis of literature data on the possibilities of using this method, which is important in clinical practice.
ORIGINAL ARTICLE
Objectives. To evaluate the informativeness of the N-terminal brain-promoting natriuretic peptide (NT-proBNP) for the diagnosis of chronic heart failure (CHF), depending on the presence of senile asthenia syndrome (SSA) in patients with arterial hypertension (AH) 80 years and older.
Materials and Methods. 320 patients with hypertension, depending on the presence of CHF and SSA, were divided into groups: group 1A — patients with hypertension, SSA and CHF (n=84), group 1B — patients with hypertension, SSA without CHF (n=77), group 2A — patients with hypertension, CHF without SSA (n=84), group 2B — patients with hypertension without CHF and without SSA (n=75). The CSA was identified by the questionnaire “Age is not a hindrance”. The level of NT-proBNP was determined in blood serum by enzyme immunoassay. ROC analysis was used to determine the threshold value of markers.
Results. In patients with hypertension and SSA without CHF, the concentration of NT-proBNP in the blood is 2.3 times higher (p=0.003) compared with patients with hypertension without SSA and without CHF, which indicates the effect of SSA on the level of NT-proBNP. In patients with hypertension and CHF without SSA, the level of NT-proBNP is 4.3 times higher compared with patients with hypertension without SSA and without CHF (p<0.001), in whom the concentration of NT-proBNP was noted below the threshold level (106.2 pg/ml). In patients with hypertension and SSA and CHF, the highest concentrations of NT-proBNP were recorded, which are 2.9 times (p<0.001) higher than in “fragile” patients with hypertension without CHF and 1.5 times higher than in “strong” patients with hypertension and CHF (p<0.001). A new threshold level of NT-proBNP has been calculated for the diagnosis of CHF in patients with hypertension and SSA aged 80 years and older — 365.9 pg/ml.
Conclusion. For the diagnosis of CHF in patients with hypertension 80 years and older without CSA, the NT-proBNP marker is informative, since, according to the data obtained, its level did not depend on the age of the patients. When using NT-proBNP to detect CHF in patients with hypertension and SSA 80 years and older, the calculated threshold marker level (365.9 pg/ml) should be used, since in these patients the concentration of NT-proBNP is increased, regardless of the presence of CHF.
Background: Osteoarthritis (OA) of the knee joint is one of the most dangerous diseases, the most significant manifestation of which is chronic pain syndrome. There is a low correlation between the radiographic stage of OA and pain progression. First of all, this is a variety of pain syndromes, among which is the pathology of periarticular structures (AS). To date, the contribution of this type to the clinical picture of OA has been sufficiently studied, primarily due to the fact that the list and frequency of these lesions have not yet been described.
Aim: to describe the basis of the main periarticular structures in patients with different radiographic stages of knee OA according to ultrasound data.
Materials and methods: The observational study has currently included 88 patients who had an outpatient appointment with a rheumatologist for knee osteoarthritis between 2021 and 2023. The study assessed 110 knee joints using clinical and ultrasound techniques.
Results: The most common periarticular ultrasound changes, regardless of radiographic stage, were pes anserine tendinopathy (57.3 %), Baker’s cyst (45.5 %), fibrosis of the severe Hoffa body (40 %) and ligamentopathy of the medial collateral ligament (36). ,4). %). A significant correlation was found between the number of changes according to ultrasound and the radiological stage (ρ=0.45 [95 % CI: 0.28, 0.59], p <0.001) as well as between the VAS and the definition of identified ultrasound changes (ρ= 0.29 [95 % CI: 0.11, p=0.002); In addition, it was shown that late stages of OA are associated with a greater content of changes (p <0.001).
Conclusion: Changes in periarticular structures are present in most patients with knee osteoarthritis; their number correlates with the VAS value and radiographic stage of OA. Details of these changes, their clinical significance and pathogenetic contribution to the progression of knee OA require further study.
ANALYSIS OF CLINICAL CASES
Fever of unknown origin is a difficult syndrome for differential diagnosis. Absence of a key feature, variety of causes and the lack of single examination algorithm makes difficult further diagnosis. The presented clinical case describes a 53-year-old patient with a prolonged fever of more than 1.5 months, pain syndrome in the facial area. During outpatient monitoring, the cause was not clarified. At the inpatient stage, a comprehensive examination was conducted for all classes of causes. The revealed changes in the thyroid gland and thyrotoxicosis made it possible to diagnose subacute thyroiditis. According to the literature, subacute thyroiditis is one of the rare causes of fever of unknown origin. Prescription of glucocorticosteroid made it possible to achieve complete regression of clinical symptoms in 4 days. After 5 months, subclinical hypothyroidism was achieved. The nosological approach and multidisciplinary interaction contributed to the correct tactics and a favorable outcome of the disease.
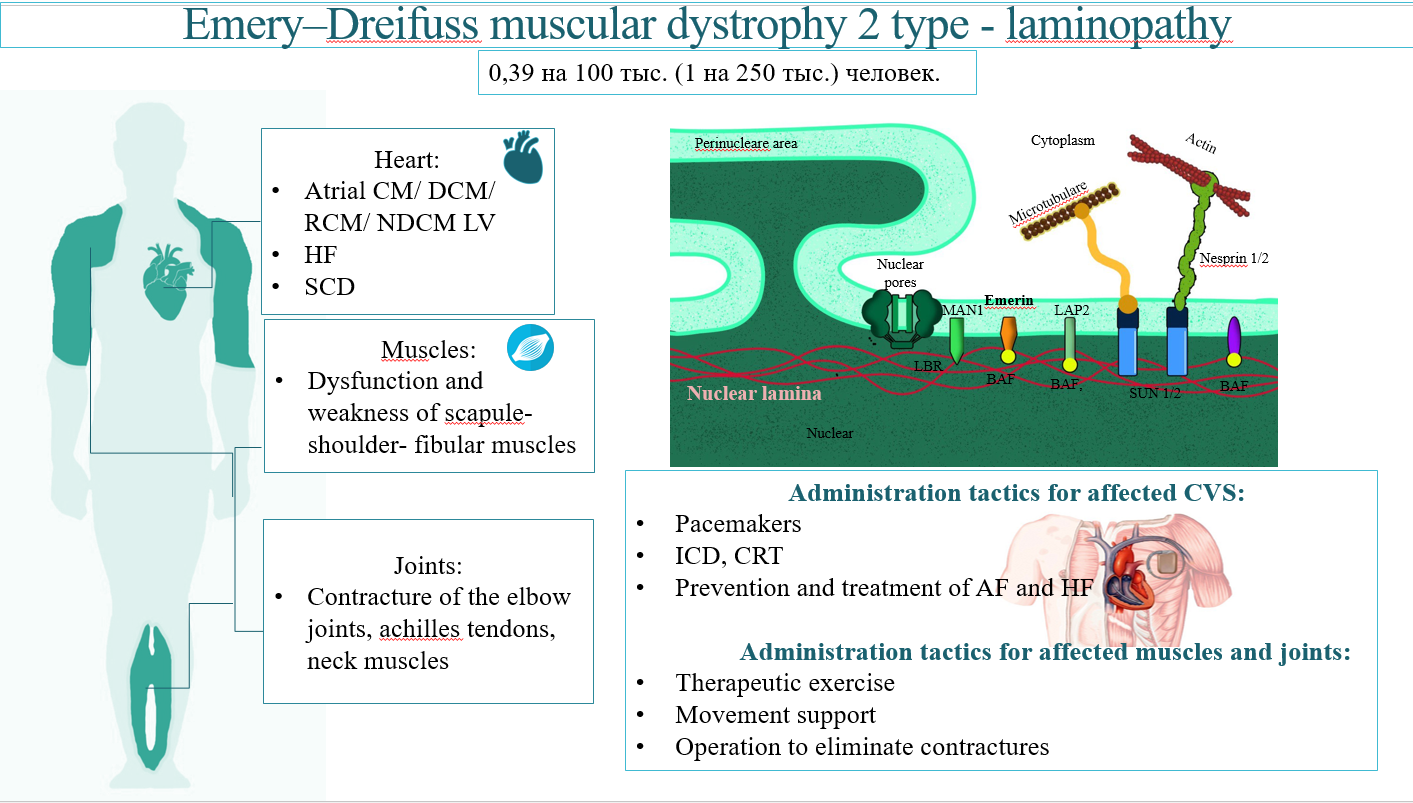
Emery-Dreifuss muscular dystrophy is a rare disease resulting from a genetic defect in nuclear envelope proteins, most commonly in emerin and lamin A/C. The disease is characterized by slowly progressing weakness of the scapular-brachial and pelvic-peroneal muscle groups, myodystrophy, primary joint contracture and cardiomyopathy with rhythm disorders and conduction abnormalities. Cardiovascular complications and life-threatening arrhythmias are the main cause of death in such patients at a young age. Depending on the leading symptoms and family history, patients are under the care of different specialists. Unfortunately, neurologists, cardiologists, cardio surgeons and orthopedics are not well informed about this rare condition and thus the disease tends to be not diagnosed in time. This article examines the data of epidemiology, pathophysiology, features of the course, diagnosis, approaches to the management of cardiovascular pathology in progressive Emery-Dreyfus muscular dystrophy with the development of LMNA cardiomyopathy. A clinical case of this disease is also given.
Kidney injury in patients infected with the human immunodeficiency virus (HIV) has a diverse spectrum. Some antiretroviral therapy (ART) drugs have nephrotoxic effects. We present a clinical case of severe combined kidney injury — chronic kidney disease (CKD) and acute kidney disease (AKD) — in a patient with HIV infection. She was on long-term treatment with a fixed-dose combination of rilpivirine, tenofovir, and emtricitabine and had normal pre-treatment renal function (estimated glomerular filtration rate 69 mL/min/1.73m2 ). There was gradual increase in blood creatinine, but the patient did not visit a nephrologist and the ART was not changed. The patient was admitted to the nephrology department two years later because she had arterial hypertension and hyperazotemia (blood creatinine 718 μmol/l). Diagnosis: chronic tubulointerstitial nephritis, CKD G5 taking into account the gradual increase in blood creatinine during long-term ART. The patient was treated with peritoneal dialysis. There was persistent decrease and stabilization of blood creatinine (210-190 μmol/l was) which indicated in AKD. The presented observation demonstrates that ART in an HIVinfected patient can lead to the development of severe combined chronic and acute kidney injury. HIV-infected patients receiving ART require regular monitoring of renal function and follow-up by a nephrologist.
ISSN 2411-6564 (Online)