REVIEW ARTICLES
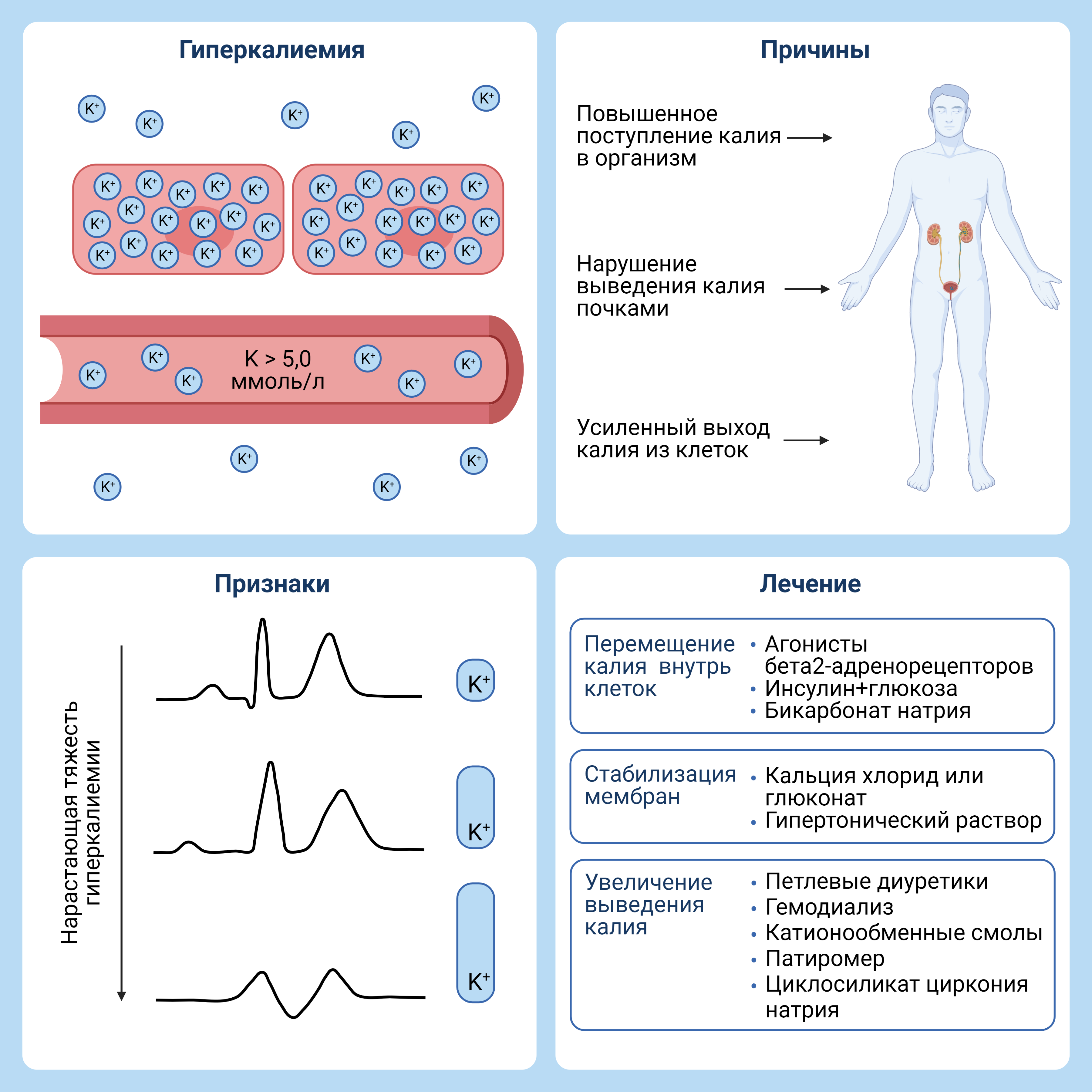
Hyperkalemia is the most common electrolyte imbalance in clinical practice. Hyperkalemia can be caused by an increased intake of potassium into the body, the shift of potassium out of cells or an abnormal renal potassium excretion. This condition is associated with a high risk of death from arrhythmias; therefore, even a slight deviation of the serum potassium level from the norm requires immediate correction. Modern approaches to the treatment of hyperkalemia include the elimination of predictors and the potassium-lowering drugs. Although inhibitors of the renin-angiotensin-aldosterone system are currently the best cardionephroprotective drugs, their administration can lead to hyperkalemia too, especially in heart failure, chronic kidney disease and diabetes mellitus. The article discusses in detail the physiology of potassium metabolism, possible predictors, prevention and treatment of hyperkalemia.
The rheumatic patients are characterized by various structural and functional changes, caused by chronic disease the necessity of constant medication intake, including anti-inflammatory drugs and immunosuppressants. In this regard, the rheumatic patients have an increased risk of intraoperative and postoperative complications. The purpose of this publication is to review current recommendations on the topic of perioperative management of rheumatic patients. The publication consists of two parts. In the first part we review the issues of perioperative administration of steroids, disease-modifying antirheumatic drugs, biologics and nonsteroidal anti-inflammatory drugs.
Epigenetics studies processes leading to changes in the activity of genes without changing the DNA sequence. Epigenetic mechanisms, such as DNA methylation and histone modifications, are formed during embryonic development, and epigenetic profiles are stably inherited in mitosis, providing cell differentiation and their further fate in the development process. Under the influence of internal and external factors such as metabolic profile, hormones, nutrition, drugs, smoking and stress, epigenetic mechanisms are actively modulated and, in this sense, a lifestyle can significantly affect the epigenome, and consequently, the gene expression profile and function of cells. It is shown that the development and function of cells of both congenital and adaptive immune systems are also regulated by epigenetic mechanisms, and negative epigenetic changes are a distinctive feature of aging and cancer. Given these data, it can be assumed that age-related changes in the profile of epigenetic labels can lead to a decrease in immune function and contribute to an increase in morbidity in the elderly. Therefore, to ensure healthy aging, better understanding of how to avoid epigenetic changes that are associated with aging of the immune system is needed. In this review, we tried to generalize the latest achievements in this field of research and consider the possibility of using them for diagnosis, prevention and treatment of diseases.
ORIGINAL ARTICLE
Obstructive sleep apnea (OSA) is a common, heterogeneous chronic disease with sleep fragmentation, metabolic and cardiovascular disorders. Continuous Positive Air Pressure (CPAP) therapy is the primary treatment for patients with OSA. However, the effects of long-term CPAP therapy with night sessions > 6 hours remain poorly understood. The aim of the study was to study the effects of different durations of night sessions of CPAP therapy on the “metabolic profile” of patients with severe OSA. Materials and methods. In a retrospective case-control study comparing two CPAP-therapy regimens by matching pairs from among patients with verified severe OSA (apnea-hypopnea index> 30/h), arterial hypertension, obesity of I-II degrees according to the WHO classification (1997), signed informed consent, 2 groups of 18 people each were formed, comparable in age, anthropometric and somnographic indicators, using CPAP therapy 4-6 hours / night and more than 6 hours / night, respectively. Patients received CPAP therapy for a year, visits were carried out at 3, 6 and 12 months. The severity of sleep apnea was verified during nighttime computed somnography (CSG) on WatchPAT-200 hardware (ItamarMedical, Israel) with original software zzzPATTMSW ver. 5.1.77.7 (ItamarMedical, Israel) by registering the main respiratory polygraphic characteristics from 11.00 PM to 7:30 AM. The optimal therapeutic level of CPAP therapy was titrated at home using devices for automatic selection of therapeutic pressure (PR System One REMstar Auto CPAP Machine with A-Flex (Philips Respironics, USA)) within 7 days after the diagnostic study. To assess the compliance of OSA patients at 3-6-12 months of CPAP-therapy, we used the original compliance analysis program Encore Pro v.2.14 (Philips Respironics, USA). Results. With the initial comparability of the groups, by the 3rd month of therapy, patients with CPAP > 6 h/night showed a statistically significant advantage over the patients with 4-6 h CPAP-therapy in ESS, neck circumference and testosterone. By the 6th month, statistically significant differences of BMI, VAI, leptin, oral glucose tolerance test, fasting insulin, HOMA-IR, lipid metabolism (HDL, LDL, triglycerides, Apo-B) appeared. By the 12th month of therapy, the CPAP group > 6 h/night had a statistically significant advantage in waist circumference, fasting blood glucose and uric acid. Differences between groups at control points persisted throughout the observation period. Conclusions. Long-term home-based CPAP therapy with sessions > 6 h/night has an advantage over therapy with sessions 4-6 h/night in achieving a rapid and pronounced improvement in metabolic profile and hormonal levels in patients with severe OSA.
Objective. To develop the pattern of early cardiovascular disorders in patients with primary hypothyroidism based on the analysis of relationship between patient’s thyroid status and some functional cardiovascular parameters depending on compensation status. Materials and methods. The examination of 163 women aged 62 [55;67] years with primary hypothyroidism was performed. The patients were divided into groups: 1 group included 54 patients aged 62.0 [57;68] years with subcompensated disease, 2 group consisted of 15 patients aged 59 [53;66] years with non-compensated disease and 3 group included 94 patients aged 63 [53;66] years with compensated hypothyroidism. Physical examination, transthoracic echocardiography, assessment of global left ventricle longitudinal strain by speckle tracking method, endothelial function and laboratory tests were performed to all patients. Regression analysis using thyroid stimulating hormone, free T4, age, duration of the disease, cause of hypothyroidism, menopause presence and natural thyroid stimulating hormone logarithm as predictors and some cardiovascular parameters of heart condition and lipid metabolism as dependent valuables was made. Results. Mathematic modeling demonstrated that the combination such factors as age, duration of disease and thyroid stimulating hormone level is the most important in left ventricle remodeling processes. However, the age only has significant influence on intima media thickness. Conclusion. Left ventricle remodeling, morphologic functional status of blood vessel wall and decrease of glomerular filtration rate are basically determined by such modified and non-modified factors as body mass index, age, duration of hypothyroidism and thyroid stimulating hormone level.
The aim: to evaluate the efficacy of respiratory muscles training in the complex treatment of patients with acute decompensated heart failure. Material and methods. A prospective randomized study included 120 patients (71 men and 49 women, mean age 73,6±5,8 years) hospitalized with acute decompensated heart failure. The main exclusion criteria were: requirement for treatment in intensive care unit; hemodynamic instability; severe pulmonary and other concomitant pathology. After initial procedures all patients were randomized to breathing exercises performed in addition to standard therapy (main group, n=60) or to standard therapy only (control group, n=60). Patients of the main group were trained in the technique of complete yogic breathing, which consists of three successive phases: abdominal, thoracic and clavicular. The participants practiced full breathing daily at least 3 times a day for 10 minutes under the supervision of instructor. The primary endpoint of the study was the change in dyspnea according to the modified Borg scale (modified by V.Yu. Mareev) on the 7th day of treatment. Results. During treatment the severity of dyspnea decreased in both groups, more significantly in the main group (from 6 (5; 6) to 3 (2; 3) points) compared to control (from 6 (5; 6) to 4 (3; 4) points, p <0,05). Significant differences between the groups were also obtained for the secondary variables of efficacy: six-minute walk distance, heart rate and breathing rate at rest, blood oxygen saturation (p ><0,05). In patients who performed breathing exercises, body weight decreased faster (0,72±0,06 kg/day versus 0,53±0,06 kg/day, p ><0,001), although the volumes of excreted fluid did not differ between the groups. In the main group moist rales in the lungs were stopped by the sixth day of hospitalization (interquartile range of 5-7 days), and in the control group — by the eighth (interquartile range of 7-9 days), p=0,024. The duration of active diuretic phase and the average daily doses of diuretics were lower in main group compared to control (p ><0,05). During hospitalization quality of life improved in both groups, more significantly in respiratory muscles training group (p ><0,01). In-hospital mortality and the rate of transfers to the intensive care unit did not differ between groups. The average hospital stay in surviving patients was significantly shorter in main group than in control (14,2±2,5 versus 17,3±2,9 days, p ><0,001). >Conclusion. Respiratory muscles training with full yogic breathing in addition to standard medical therapy for patients with acute decompensated heart failure leads to a more significant reduction in the severity dyspnea, increased exercise tolerance, improved blood oxygen saturation, and reduced need for diuretics. The use of full breathing is associated with significant improvement in the quality of life and decrease in the length of hospital stay, but does not lead to improvement in hospital outcomes.
ANALYSIS OF CLINICAL CASES
In early 2020, the World Health Organization announced the emergence of the disease-a new coronavirus infection (COVID-19). High contagiousness and asymptomatic transmission of the virus led to a rapid spread of infection and reached the scale of a pandemic. It was found that the SARSCoV-2 virus is pathogenic to the lower respiratory tract. At the same time, there are extrapulmonary manifestations, including skin rashes, which are characterized by an extreme variety. Some authors describe skin lesions as the first, and sometimes the only, symptom of a new coronavirus infection. Thus, skin manifestations should be carefully evaluated by dermatologists during the examination, especially during the ongoing pandemic.
This article presents 6 clinical cases with various skin manifestations in the acute period of COVID-19 infection. The first patients to complain were dermatologists. Rashes on the skin are characterized by a variety and prevalence: polymorphic vasculitis, livedo-angiitis, urticary, spot-papular, papu lo-vesicular, papulo-squamous elements. All cases are united by the presence of the main symptoms of coronavirus infection characteristic of the acute period — hyperthermia, headache, fatigue, myalgia, partial or complete anosmia, ageusia.
Thus, the exchange of clinical experience of skin manifestations in COVID-19 infection is extremely relevant during the ongoing pandemic. The analysis of the accumulated data will provide an understanding of the diagnostic significance and the ability to assess the prognosis when observing such patients.
ISSN 2411-6564 (Online)