LECTURES
Examination of the skin is a widely available and simple method of examining the patient, which nevertheless allows you to diagnose systemic disorders and diseases in the human body at an early stage. A doctor of any specialty may encounter dermatological paraneoplastic syndromes in his practice, which are a group of skin diseases associated with malignant neoplasms, but not directly related to the primary tumor or its metastases. Timely analysis of dermatological paraneoplastic syndromes makes it possible to suspect malignant tumors that cause them and urgently refer the patient to an oncologist for the purpose of early diagnosis and treatment of a potentially curable oncological disease. In clinical practice, paraneoplastic Leser-Trélat syndrome is very common, which is manifested by the sudden appearance of multiple seborrheic keratomas (mainly in the back and abdomen) and an increase in their number and size over a short period of time (weeks, months). Treatment of this syndrome can be carried out both simultaneously and after treatment of the underlying malignant disease. Dermatological paraneoplastic syndromes require further in-depth study to understand the pathogenesis, create a clear classification and develop algorithms for the doctor’s actions in case of their detection.
REVIEW ARTICLES
In 2020, a consensus document of the European Society of Cardiology on the management of patients with myocardial ischemia with non-obstructive coronary arteries was released. The main provisions of the new document are aimed at identifying a special group of patients with chronic coronary syndrome and suspected vasospastic or microvascular angina in order to rationalize and personalize the approach to their management. Most patients with established myocardial ischemia do not have obstructive coronary arteries when undergoing coronary angiography. Coronary microvascular dysfunction and epicardial vasospasm, alone or in combination with obstructive coronary artery atherosclerosis, are the causes of myocardial ischemia. In this case, microvascular dysfunction is considered as a significant provoking factor in the pathogenesis of refractory angina pectoris. Diagnosis of such conditions is often difficult, and therefore the correct therapy is not prescribed for such patients. As a consequence, these patients have a poor quality of life, which leads to hospital readmissions, poor cardiovascular outcomes in the short and long term, and a significant burden on health care resources. The article discusses the possibilities of applying new recommendations and consensus in the diagnosis and management of such patients in outpatient clinical practice in Russia. At the initial stages of diagnosis, priority is given to non-invasive research methods; in-depth examination, carried out using invasive methods with a pharmacological testing. Patient management uses a stepwise strategy depending on the specific clinical situation. Calcium channel blockers or beta blockers remain the first line anti-ischemic therapy.
The gut microbiome is a variable system that not only adapts to signals and information coming from humans, but also affects its host due to a complex system of interactions of living microorganisms, phages, viruses, plasmids, mobile genetic elements, molecules synthesized by microorganisms, including their structural elements (nucleic acids, proteins, lipids, polysaccharides), metabolites (signaling molecules, toxins, organic and inorganic molecules) and molecules synthesized by the human body. Modification or modulation of the microbiome by correcting the diet, the intensity of physical activity, the appointment of components of personalized products (prebiotics, probiotics, paraprobiotics, postbiotics, autoprobiotics) can lead to changes in species diversity, the metabolic profile of the intestinal microbiome and the regulation of metabolic processes, local and systemic response to infectious diseases, drug metabolism, the activity of many organs and systems due to the presence of physiological axes “gut microbiome–central nervous system”, “gut microbiome–liver”, “gut microbiome–kidneys” and some others. New, targeted directions of modification of the intestinal microbiome are being studied, which consist in targeted exposure to pathogenic microorganisms, including intracellular and resistant to antibacterial drugs.
The dynamic nature of the intestinal microbiome, the ability to change and adapt under the influence of some of the studied factors opens up new promising areas of medical prevention and treatment of somatic and mental diseases. Undoubtedly, the modification of the microbiome for clinical purposes is aimed at improving human health. However, individual, not always predictable, changes in the microbiome in response to modifying factors may be due to the uniqueness of the species composition and functional potential of microorganisms in each person.
Due to the high morbidity and mortality, the problem of severe alcoholic hepatitis has not lost its relevance to date. In the absence of specific therapy, the associated to him one-month survival rate is low, and mortality rates reach 30-50 %. Although the use of corticosteroids is a scientifically proven first-line treatment for severe alcoholic hepatitis, a short-term response is observed in approximately 60 % of patients with no long-term survival benefits compared to placebo. It should also take into account the occurrence of adverse side reactions to their use in about 50 % of patients, as well as the risk of complications, in particular, bacterial and fungal infections. The second-line drugs, for example, pentoxifylline, etanercept, infliximab, N-acetylcysteine, etc. in severe alcoholic hepatitis did not show an improvement in the clinical outcome. The modern guidelines discuss the feasibility of liver transplantation in carefully selected patients who do not respond to corticosteroid treatment with severe alcoholic hepatitis. Nevertheless, due to numerous contradictions, it is too early to talk about the introduction of this approach into clinical practice. In recent years, some progress has been made in understanding the pathophysiological mechanisms of the development of alcoholic hepatitis, which served as an impetus for new directions of its pathogenetic therapy. One of them is the techniques that provide intestinal eubiosis, in particular, through the fecal microbiota transplantation. The purpose of the review was to describe the pathophysiological prerequisites and therapeutic potential of fecal microbiota transplantation from healthy donors to patients with severe alcoholic hepatitis. Experimental studies have shown a positive effect of fecal microbiota transplantation on the intestinal microflora, which led to a weakening of alcohol-induced liver damage. In patients with severe alcoholic hepatitis, it improved the severity of its symptoms and contributed to increased survival compared to those receiving corticosteroids. These preliminary results are encouraging and create conditions for further clinical trials involving a large cohort of patients with severe alcoholic hepatitis, which will allow us to identify those for whom fecal microbiota transplantation will be most effective with minimal risk of complications.
The article briefly summarizes recent advances in genetic medicine that paved the way for the further development of gene therapy and set the stage for the development of next generation technology. Issues related to the main obstacle for wider application of gene therapy methods, in particular, with the immune response to gene delivery vectors and transgene products are considered. In this context, the role of new technology allowing to bypass the immune obstacle, such as development of modified capsids of adeno-associated viruses (AAV) and methods for temporary removal of antibodies from the bloodstream, as well as gene transfer into tissues using nanoparticles, is discussed. Along with the technology of the first generation gene therapy focused on the delivery of transgenes into target tissues, latest advances in the development of a completely new approach to gene therapy which is based on precise modification of the human genome sequence, gene editing technology, are summarized. Finally, promising next-generation gene editing technology is outlined, such as RNA-targeted editing technology and epigenome editing technology, which are more specific, precise, efficient and applicable to different groups of diseases. The article concludes that gene therapy and, in particular, human genome editing is perhaps the most exciting and revolutionary biotechnology of our time, due to both recent developments and opportunities it might provide in the nearest future.
The problem of the formation of irreversible residual changes after suffering viral lung damage with COVID-19 (COronaVIrus Disease 2019) after two years of the pandemic remains important and discussed. This is due to a large number of patients who have had a coronavirus infection (including those with a large amount of lung damage) and a possible unfavorable prognosis with a decrease in the quality and life expectancy. Given the fact that antifibrotic therapy has recently been actively used for a number of interstitial lung diseases (with idiopathic pulmonary fibrosis and systemic diseases), the question of the possible use of these drugs in case of an unfavorable outcome of COVID-19 is being considered. However, it is still not known exactly how often fibrosis develops in the outcome of a new coronavirus infection, and groups of patients who may have a poor prognosis in the form of an outcome in fibrosis have not been clearly identified.
The review considers the pathogenetic aspects of the possible development of irreversible changes in patients with COVID-19, predisposing factors, as well as diagnostic features with an emphasis on CT scan with the authors’ own observations.
ORIGINAL ARTICLE
Aim: To assess the likelihood of developing heart failure during a three-year prospective follow-up and develop a method for its comprehensive assessment in individuals with atherosclerotic lesions of various vascular beds. Materials and methods: The study included 519 patients with atherosclerotic lesions of various vascular regions, of which 360 (69.4 %) were men, 159 (30.6 %) were women (mean age 60.0±8.7 years). Results: Analysis of the likelihood of developing heart failure clearly demonstrated that factors such as the value of the ejection fraction, % (p = 0.040), the value of the base of the aorta, mm. (p = 0.049), the degree of atherosclerotic lesions of the left coronary artery trunk,% (p = 0.013) and the severity of posterior lateral branch stenosis,% (p = 0.048) influenced the risk of developing the discussed endpoint in the long-term period in patients with peripheral atherosclerosis. Conclusions: The probability of developing vascular events and adverse outcomes during a three-year prospective followup was assessed. It was found that hospitalization for heart failure over a three-year period occurred in 3.4 % of patients with atherosclerotic lesions of various vascular beds and their combinations. It is noted that such groups of factors as “the value of the ejection fraction% + the value of the base of the aorta, mm.” (p=0.025), “the degree of atherosclerotic lesions of the posterior lateral branch, % + the value of the ejection fraction, %” (p=0.046), influenced the risk of developing heart failure in the long-term period in the subjects of the survey group. Using logistic regression equations, original prognosis tables have been developed that provide information on the likelihood of developing heart failure, which can be used in real clinical practice in patients with peripheral atherosclerosis.
ANALYSIS OF CLINICAL CASES
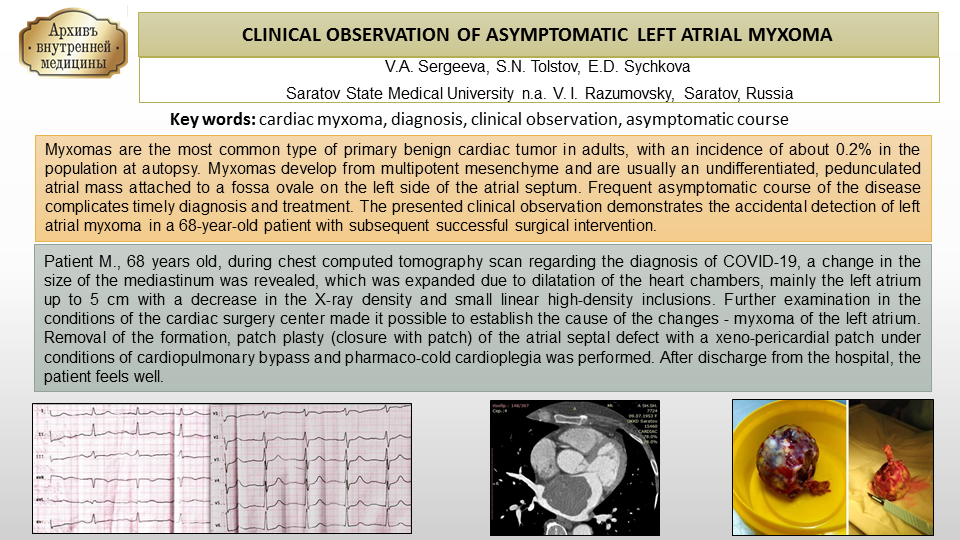
Myxomas are the most common type of primary benign cardiac tumor in adults, with an incidence of about 0.2 % in the population at autopsy. Myxomas develop from multipotent mesenchyme and are usually an undifferentiated, pedunculated atrial mass attached to a fossa ovale on the left side of the atrial septum. Frequent asymptomatic course of the disease complicates timely diagnosis and treatment. The presented clinical observation demonstrates the accidental detection of left atrial myxoma in a 68-year-old patient with subsequent successful surgical intervention.
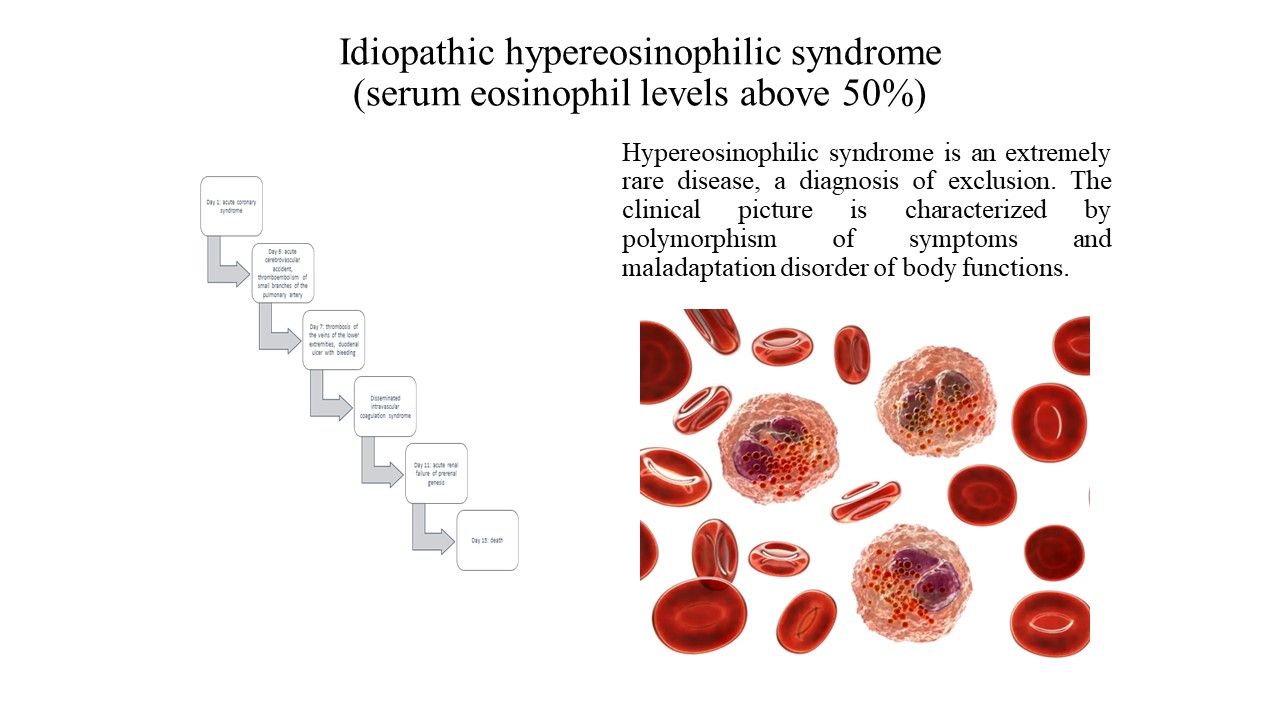
Idiopathic hypereosinophilic syndrome is a rare phenomenon in medical practice. The main criterion for diagnosis is a persistent increase in the level of eosinophils above 1.5 * 109/ l in the blood serum and the absence of clinical and laboratory and instrumental data explaining the possible nature of this condition.
A clinical case of idiopathic hypereosinophilic syndrome, which occurs under the guise of acute coronary syndrome, is presented. A detailed analysis of this case was carried out in order to highlight a possible variant of the course of this disease, as well as to increase alertness in the area of “large” eosinophilia.
ISSN 2411-6564 (Online)